Article
Risks in Surgery: Primary Allegations

What’s My Risk?
Primary Allegations in Medical Malpractice Claims Against Surgeons: How to Protect Your Patients and Yourself
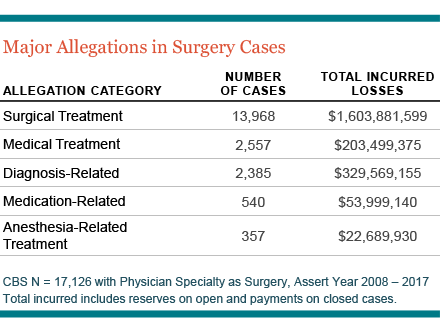
As a surgeon, every time you step into the operating room (OR), you run the risk that something could go wrong. According to national Candello Data (previously known as CBS), more than 75 percent of all malpractice complaints against surgeons (13,168 out of 17,126 total) over a 10-year period listed surgical treatment as the primary allegation. These led to more than $1.6B in losses.
CRICO’s findings, which are based on 30 percent of all medical professional liability (MPL) cases across the United States, are particularly concerning since incidents involving surgeons often have devastating outcomes, commonly involving death, or high-severity injuries related to nerve damage, perforations, or punctures.
With so much at stake, it’s crucial to understand your biggest areas of vulnerability so you can take steps to mitigate the risks to yourself and your patients.
Risks throughout the Surgical Process
When it comes to primary allegations against surgeons, the majority of cases are centered around intra-operative technical errors; yet surgical errors certainly aren’t limited to the OR; they can also happen before and after treatment. And, often, it is a cascade of events or oversights that unfold throughout the entire treatment process that ultimately results in harm to the patient and puts you at jeopardy of being sued.
Some of the preventable errors that may transpire include misdiagnosing patients and/or not selecting the most effective type of surgery, not adequately explaining the risks involved, demonstrating weak clinical judgment, using poor technical performance during an ambulatory or inpatient procedure, and not communicating clearly with other team members at any point (or multiple points) of the patient journey.
Areas for Malpractice Risks
Paying attention to the areas where the greatest risks exist—and taking steps to address your weaknesses at every stage of the surgical process—can help prevent a negative outcome.
Intra-operative risks: The crowded and stress-filled operating arena is rife with opportunities for things to go wrong. In fact, with so much coordination required among surgeons, residents, technicians, anesthesiologists, and nurses, a high degree of coordination and team work is essential to prevent technical errors and miscommunication.
Outpatient surgery risks: With outpatient surgical procedures becoming more common, there is more demand for the ambulatory OR and, thus, increased chance for errors and injuries to occur. Inadequate credentialing, protocols, systems, and staffing to respond to complications during an outpatient surgery procedure can put patient safety at risk and make providers vulnerable to being named in a malpractice suit.
Never events: In both inpatient and outpatient surgeries, the threat of never events is a serious concern. From operating on the wrong patient or performing the wrong procedure, to failing to remove foreign objects, these inexcusable incidents put patients and surgeons at extreme risk of negative consequences.
Post-operative risks: When patients are moved to a new team of caregivers following surgery, critical information can be missed during a poorly managed handoff. When pertinent surgical information is not clearly shared with the care team and other providers life-threatening adverse reactions can be missed.

Opportunities for Improvement
The best way to protect yourself is to adopt strategies that can improve your safety profile. For instance:
- Participate in simulation-based training that offers surgical teams a valuable opportunity to practice the latest operating techniques. This allows you to anticipate areas where things could go wrong and determine how best to head them off.
- Take advantage of intra-operative technical coaching, where an accomplished colleague watches you perform surgery either live or over video and provides notes and feedback on safety behavior and teamwork skills.
- Develop an OR crisis checklist that describes what to do during a variety of clinical crises. By having this document on hand, members of your surgical team will have guidance so they don’t overlook any critical steps.
- Insist on standardized communication in order to provide a common language that everyone will understand and a common structure through which to communicate clearly and respectfully so nothing falls through the cracks.
- Promote effective handoff practices that prioritize an interdisciplinary team-based approach wherever possible and minimize reliance on patients and family to convey key information to providers.
Making Key Changes
CRICO’s MPL data paints a clear picture of the importance of focusing on these and other areas to improve your safety practices. You can also tap into CRICO’s many resources, which can help you address your biggest vulnerabilities in order to ensure the very best outcomes for everyone involved.
Learn More
- 2018 Candello Report: Medical Malpractice in America
- Surgery: Attending Notification Guideline
- Malpractice Risks in Surgery: 2009 CRICO Strategies National CBS Report
- Surgical Case Studies
Related Articles
Risks in General Medicine: Contributing Factors


Risks in Surgery: Contributing Factors

What’s My Risk Library

