Newsletter
What Keeps “My Doctor” Up at Night
Jan 29, 2015
Generally, an office-based primary care physician (PCP) is whom a patient identifies as “my doctor.” In the ambulatory setting, however, providing the safest care possible for everyone who thinks of you as “my doctor” presents unique challenges. Amidst the normal distractions and interruptions (some call it chaos), PCPs and other caregivers have to navigate myriad factors that can contribute to the risk of error.
Click the play button to jump to the excerpt of Dr. John Ingard discussing issues that occupy his mind on a given day. Click "YouTube" to view this directly in a larger screen. View full podcast >>
When a practice operating under such challenges lacks a systematic approach: to diagnosis, to test or referral management, to patient follow up, etc., the risk of patient harm is exacerbated. But PCPs looking for guidance to improve and streamline processes are likely to find high variability in the resources available—and minimal connectedness with their sponsoring institutions.
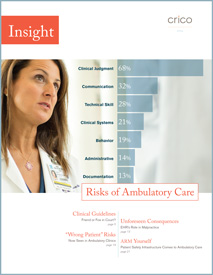
With the limited resources that most primary care practices have available to apply to patient safety, focal points are essential. Through retrospective analysis of medical malpractice data and forward-looking discussions about day-to-day concerns, CRICO has identified the five most pressing areas of risk for ambulatory caregivers:
- cognitive vulnerabilities (too little time with patients, inadequate consultation relationships);
- systems-related impediments (handoffs, bulky/non-integrated systems, communication breakdowns);
- a complex practice environment isolated from a programmatic patient safety support structure;
- lack of robust information technology solutions; and
- the worry that the amalgamation of these factors increases the risk of missing a diagnosis or mishandling a treatment protocol.
Click the play button to jump to the excerpt of Dr. Gila Kriegel talking about Ambulatory Risk. Click "YouTube" to view this directly in a larger screen. View full podcast >>
To determine what concerns present the biggest risk and which interventions produce the biggest reward, each practice has to define the key characteristics of a safe, efficient, and enjoyable environment for patient and providers. For example, a practice that affords PCPs and their patients the safest possible care is one in which:
- Providers have time, tools, and fail-safe systems to ensure appropriate levels of care across their full patient panel.
- Teamwork is honored and optimized within the practice and across the medical neighborhood.
- Providers use data, quality improvement tools, and safety intervention techniques to identify and tackle the problems that are unique to their environment.
- Patients are engaged partners in their care and treatment.
Whether or not your colleagues agree with this example, taking the time to articulate the key characteristics that define your ideal practice environment is a valuable first step in being the “my doctor” your patients expect.
Additional Material
- Ambulatory Risk Manager Grant Program
- Insight Into Risks In Ambulatory Care
Latest News from CRICO
Ambulatory Safety Nets: Protecting Providers and Promoting Safety with Systems to Reduce Delayed Cancer Diagnoses

Developing a Framework and Electronic Tool for Communicating Diagnostic Uncertainty in Primary Care: A Qualitative Study

Surgeon’s Coaching Techniques in the Surgical Coaching for Operative Performance Enhancement (SCOPE) Program

