Case Study
Missed Opportunities in the ED
Description
A four-year-old boy required emergency surgery and removal of 12 inches of necrotic bowel 10 hours after arriving in the emergency department (ED) with tell-tale symptoms.
Key Lessons
- A diagnosis can be delayed if multiple indicators are understood by multiple caregivers, but not collectively by any one of them.
- Supervision of trainees of varying experience levels requires an understanding of who is backing up whom.
- Numerous small errors or omissions can align to create a disaster.
Clinical Sequence
At 12:30 p.m., Tuesday, a four-year-old boy with a history of surgical repair of a volvulus (at age two) was brought to the emergency department (ED) due to increased lethargy, bilious vomiting for 18 hours, and constipation for two days. On admission, the patient was afebrile, his pulse was 180, and his respiratory rate was 44. The white blood count was 2.4, with a shift to the left; BUN was 27 with a serum bicarbonate level of 20.
At 2:00 p.m., the ED flow sheet stated “awaiting general surgical consult.”
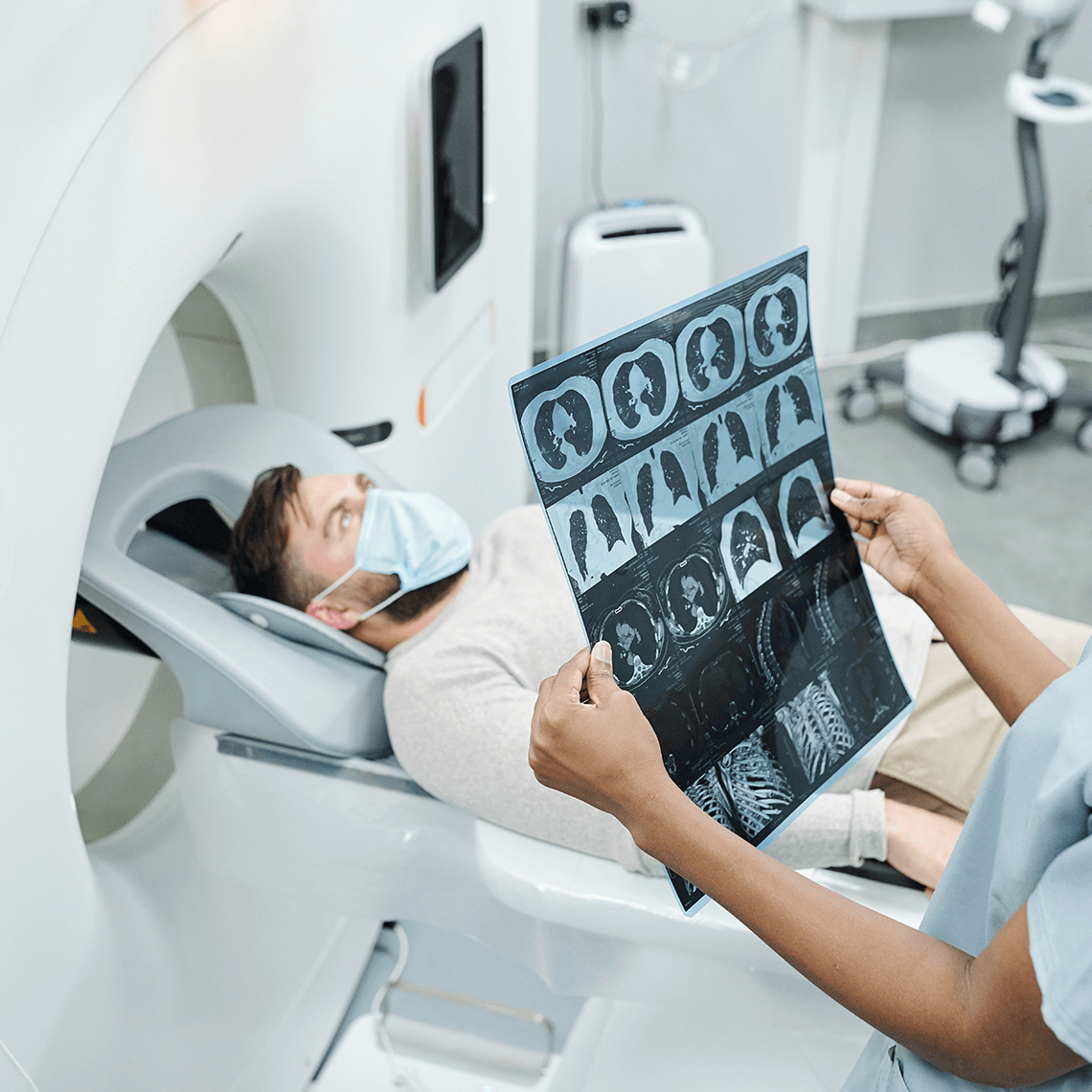
At 3:30 pm, KUB films showed “dilated loops of bowel, which may represent a partial or early small bowel obstruction.” Placement of a nasogastric tube immediately drained 400cc of bilious fluid. The patient was given two boluses of 250cc of normal saline, followed by five percent dextrose in half normal saline at 40cc per hour. The child was diagnosed with “partial small bowel obstruction” and was admitted to the surgical service.
At 4:00 p.m., the patient was seen by a surgical intern (PGY1). She took the X-rays to the attending surgeon of record (who was in the operating room with another patient) and his surgical assistant, a fourth-year general surgery resident. The attending, who had performed this child’s first surgery two years prior, and the resident agreed that the films showed a partial small bowel obstruction. The attending ordered that IV fluids be continued, that additional labs be ordered, that an additional KUB be obtained at 7:00 p.m., and that an infectious disease consult see the child once he was moved to a surgical floor (which occurred around 6:00 p.m.).
At 6:00 p.m., when the attending surgeon finished his prior case, and just prior to his leaving the hospital for the day, he asked the fourth-year resident to see the boy with the bowel obstruction.
At 6:30 p.m., the resident found the patient’s abdomen non-distended with no signs of peritonitis. She ordered that the repeat KUB and labs be obtained then, rather than 7:00 p.m. She was aware that the blood count had a shift to the left.
At 6:45 p.m., the KUB films showed a worsening small bowel dilatation consistent with a small bowel obstruction (Radiology’s official read would be Wednesday morning). At 7:00 p.m., the resident phoned the attending surgeon with the results of her exam: she believed that the patient looked stable, but had not yet seen the repeat X-rays.
From 7:00-9:00 p.m., the general surgery resident was on evening rounds and, thus, did not see the 6:45 film.
At 9:00 p.m., a nurse notified the resident that the child did not look right and he was not responding to a needle stick. The resident left rounds and found the child lethargic, with a heart rate in the 180s.
At 9:45 p.m. the general surgery resident then asked the senior resident (a pediatric surgical fellow) to see the patient. He ordered a third set of films (the child fainted in X- ray), which showed more clearly that a closed loop obstruction had occurred, and contacted the on-call surgeon.
At 10:15 p.m., the on-call surgeon prepped for emergency surgery. Antibiotic therapy was instituted and the patient was taken to the OR around 10:45 p.m. A 12-inch segment of dead bowel had to be removed. During surgery, the patient suffered cardiovascular collapse, lost his aortic pulse, and had to be resuscitated via CPR. The post-operative course was complicated by hypotension due to overwhelming sepsis and terminal shock. ECMO (heart-lung machine) was required to keep the child alive.
Allegation
The patient’s parents filed a malpractice claim against the attending surgeon and the general surgery resident alleging that their inactions resulted in a delayed diagnosis, unnecessary bowel damage, and complications related to the emergency surgery.
Disposition
The claim was settled in excess of $1 million, with 60 percent allocated against the attending and 40 percent against the general surgery resident.
Analysis
Vulnerabilities
- The patient was at increased risk for bowel obstruction of adhesions due to previous surgery.
- At 12:30 p.m., the patient’s test results—WBC 2.4 with a left shift: a sign of infection, abnormal X-ray—were not fully appreciated as signs of potentially dead or severely compromised bowel.
- The surgery consult ordered at 2:00 p.m. did not occur until 6:30 p.m.
- Abnormal X-rays, which showed a loop of bowel that was highly suggestive of closed loop obstruction, did not prompt quicker attention by an attending or senior resident.
- The patient was admitted to the surgical service without a surgical consult.
- After the parents received assurances that the attending surgeon would examine their son, the senior surgeon left the hospital without either seeing him personally or arranging for someone with sufficient experience and training to make sure that emergent surgery was not required.
- The patient maintained a pulse of 180-188 after six hours of vigorous hydration.
- At 6:30 p.m., the general surgery resident underestimated the situation when she examined the patient; she ordered a KUB and blood work on an urgent basis but did not review the test results for two hours (because she was on rounds).
- Vital signs were not checked on a regular basis.
- The general surgery resident did not consult the senior resident until 9:45 p.m.
- Antibiotics were not given until 10:30 p.m. in the OR.
- No one from the surgical team was notified of the radiology film results.
Recommendations
This case clearly exposed numerous vulnerabilities in the areas of supervision, communication of critical test results, and patient monitoring (among others). As with most adverse medical events, this case was the result of a constellation of decisions (or omissions) that, individually, were not necessarily egregious, but together spelled disaster.
The role of systems and protocols is to prevent those individual missteps from aligning in such a way that the patient is exposed to harm. Unfortunately, what specifically needs to be prevented is often only uncovered when something goes tragically wrong. Fortunately, health care leaders understand the unique value of malpractice cases and near misses as opportunities for improvement. Through root cause analysis and other dissective techniques, clinicians and administrators can pinpoint the vulnerabilities in their processes and workflow, and develop strategies to reduce the risk of recurrence.
As a direct result of this case, changes have been introduced that will protect future patients and keep clinicians out of court and in practice.
This is a fictitious case that illustrates commonly encountered issues and is for educational purposes only. Any resemblance to real persons, living or dead, is purely coincidental.
See More MPL Cases
Medication Mix-up Contributes to Patient’s Death
Incidental Does Not Mean Insignificant
When Test Results Go Unspoken