Article
Follow up and Coordination
 According to CRICO’s 2014 Candello Benchmarking Report: Malpractice Risks in the Diagnostic Process, errors at any step in the diagnostic process can misdirect providers in the later stages if they rely on myopic thinking or inaccurate findings. As a preliminary diagnosis is pursued, some evidence may support it, some might not. By the time someone on the patient’s care team reaches a “let’s start again” point, there is momentum behind the preliminary diagnosis that has to be slowed or redirected.
According to CRICO’s 2014 Candello Benchmarking Report: Malpractice Risks in the Diagnostic Process, errors at any step in the diagnostic process can misdirect providers in the later stages if they rely on myopic thinking or inaccurate findings. As a preliminary diagnosis is pursued, some evidence may support it, some might not. By the time someone on the patient’s care team reaches a “let’s start again” point, there is momentum behind the preliminary diagnosis that has to be slowed or redirected.
For many patients with an undetermined condition, the diagnostic process is non-linear. Assessment leads to testing that leads to consults that lead to more assessment and testing—sometimes spread out over weeks or months. As one possible diagnosis is ruled out, the process backs up a step or two or three, and proceeds down an alternate path. With each new interaction between the patient and the system, with each new referral or test result, comes opportunities for breakdowns in the communication of critical information and gaps in the coordination of care across an expanding list of providers.
In outpatient settings, care coordination becomes even more challenging than it is in the confines of a hospital. Patients have to communicate to multiple clinicians, clinicians have to communicate with each other, electronic systems may or may not communicate across platforms. Patients are being asked to be more engaged in their care, but that doesn’t mean they should have to carry the entire burden. An individual who doesn’t feel well, who is anxious to know why, and who has sat in multiple waiting rooms for tests and exams, needs caregivers and health care systems to maintain vigilance throughout an accurate diagnosis and the initiation of a care plan. Physicians—and the other clinicians who see the patient during his or her diagnostic journey—are less vulnerable to errors when they are clear about which individual provider is coordinating the patient’s course. Patients are less vulnerable when the coordinating provider clearly communicates test results, follow-up steps, and (if appropriate) a treatment plan.
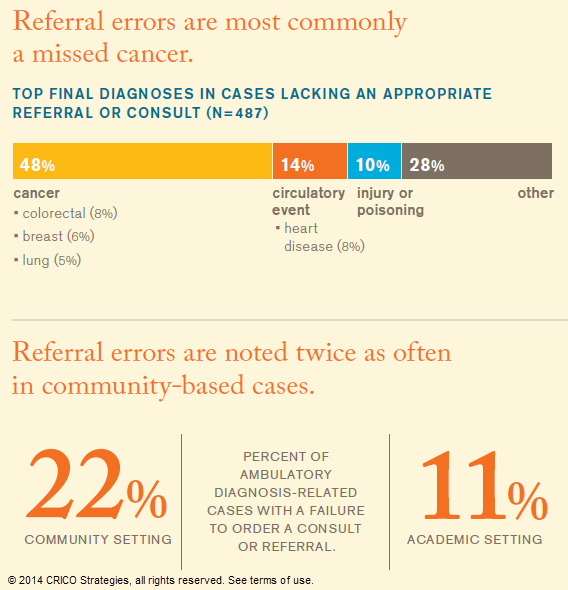
Analysis of cases that fall under this stage of the diagnostic process indicate that decisions, documentation, and communication related to consultative support significantly impacts diagnostic success. Well-coordinated care with timely consults and comprehensive communication will most likely raise awareness of unresolved concerns and redirect the cognitive process. On the other hand, even a diagnostic process along the correct path can be impeded or misdirected if the providers responsible for confirming the diagnosis and establishing a care plan fall short or leave issues unresolved and unassigned.
Dr. Mark Graber discusses ways to improve follow up. (32 sec)
This page is an excerpt of the full Candello report: Malpractice Risks in the Diagnostic Process.
Diagnostic Process Report Contents

What Experts are Saying
“As a caring physician and humble diagnostician, I’m interested in knowing when I’m wrong and what I can do better. I want to be able to acknowledge uncertainty, so I can say to the patient:
It’s not always easy to sort out with certainty every patient with headaches (or chest pain, etc.). It doesn’t look like you have anything serious, but let’s keep the door open, and feel free to call me if you’re not getting better.
Practicing this way requires creating a safe space for me and my colleagues to look for, and learn from errors. It means creating an atmosphere where I am not afraid of losing my job if I make a wrong diagnosis, as we all inevitably do.
Instead, we need a culture where each person on the team is highly respectful, and feels like we’re all in this together and is not afraid to admit or share errors.”

Gordon D. Schiff, MD
Brigham and Women's Hospital
Related Articles
Documentation Dos and Don’ts
PCPs Miss Chances with MIs