Case Study
Pre-op Findings Could Have Prevented Extra Surgeries
Allegation
The patient sued the insured facility for failure to identify and remove the gallstone in the distal common bile duct, requiring additional procedures.
Clinical Sequence
On 9/17, a 21-year-old female presented to her local ED with complaints of upper abdominal pain. Ultrasound revealed multiple stones in the gallbladder without evidence of wall thickening. It was also noted that the common bile duct appeared normal. A cholecystectomy was scheduled for 9/21.
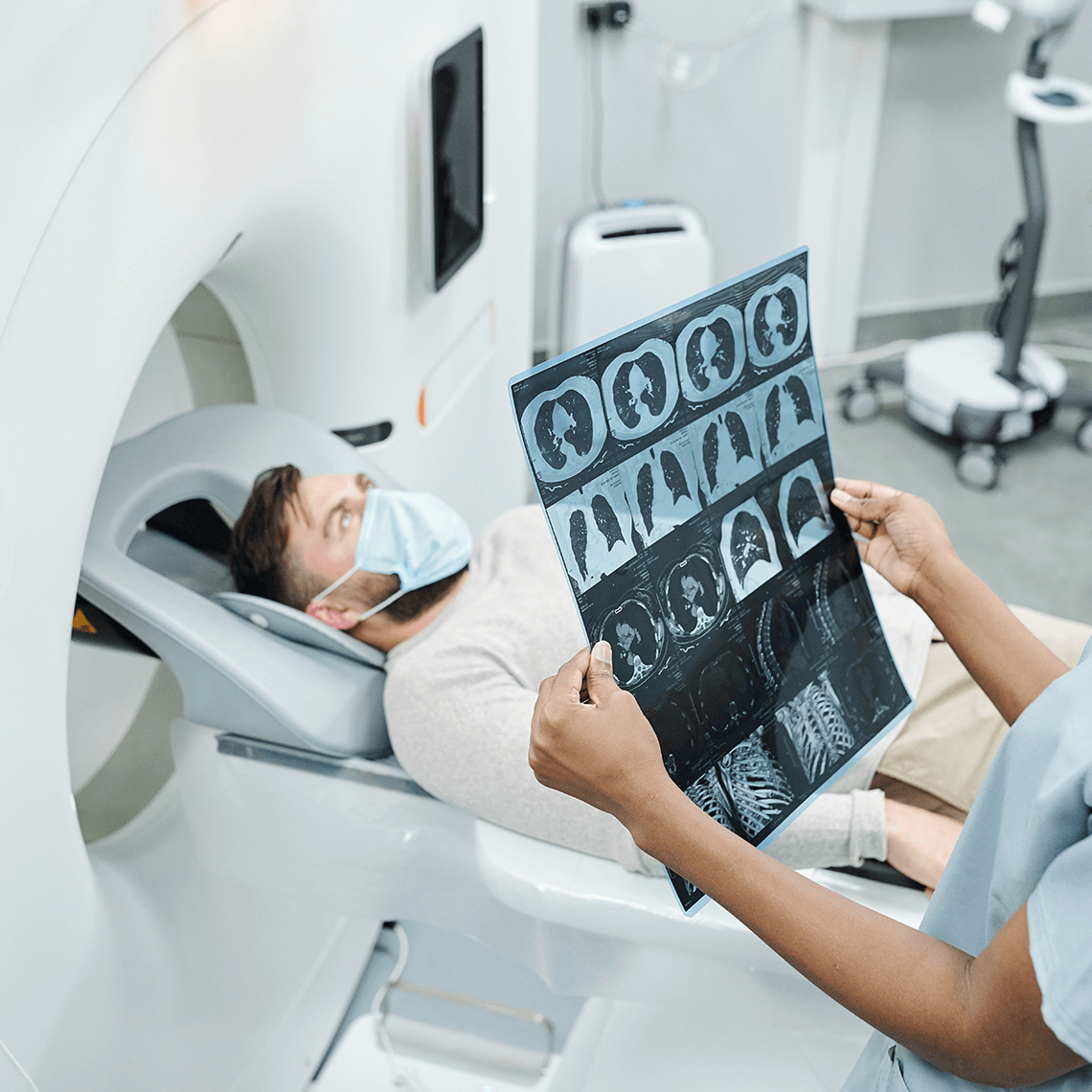
A day after the ED visit, the patient returned with severe pain. An abdominal x-ray confirmed the presence of stones in her gallbladder, as seen the previous day on ultrasound, but it also revealed an additional stone outside the gallbladder in the common bile duct. The new findings were discussed with the surgical resident the next day.
Surgery was performed on 9/21 as planned, and was uneventful. The operative report contained no mention of a stone outside the gallbladder.
On 9/30, the patient had returned to school and she presented to a different facility to be evaluated for jaundice. An abdominal CT revealed biliary dilation and a large calcified stone in the distal common bile duct. The patient required two endoscopic retrograde cholangiopancreatography (ERCP) procedures under anesthesia to address the stone. She recovered without further problems. The original surgeon met with the patient and her family to disclose and apologize for the miscommunication that occurred prior to the first surgery. Because of the disclosure and sympathy exhibited by the surgeon, the family only requested compensation for expenses.
Key Lessons
- A reliable system to reconcile and communicate serious findings from imaging studies is essential to safe, high quality care.
- A pre-op briefing allows an opportunity for the surgeon to review the patient’s file and any recent relevant testing that was done.
- Timely disclosure and apology in a caring manner can help mitigate the consequences of an error.
Description
A young woman underwent two unnecessary procedures when x-ray findings of an additional calcified stone in the common bile duct two days prior to his scheduled cholecystectomy were never communicated to the attending surgeon.
Analysis
Clinical Perspective
- The attending surgeon was unaware of the additional stone seen on the pre-op x-ray.
Hospital protocols and guidelines help ensure a reliable system for giving and receiving important study findings. Adherence to such protocols by junior staff who may not recognize the full implications of some findings—as well as by the senior attendings who can ask if new studies exist before proceeding with treatment —helps ensure that critical changes in care plans occur for every patient in a timely way.
Patient Perspective
- The patient trusted that important clinical findings would be reviewed and considered before her surgery proceeded. She was upset that she required two additional procedures, seemingly unnecessarily.
Although relaying information in large, complex organizations is very difficult, patients often expect institutions to do it right every time, for every patient when it matters. An honest disclosure when information slips through the cracks and causes a problem—delivered by a caring clinician—can help mitigate the resentment.
Risk Management Perspective
- The resident did not share a significant finding with the attending surgeon prior to surgery
Sometimes residents simply don’t understand the relevance of the finding and therefore the need to notify the attending. Or they may hesitate to volunteer information of questionable value if the work culture is intimidating. Team training can help flatten a hierarchy that threatens patient safety by shutting down communication between providers. Encouraging information flow among team members at varying levels of seniority can counter that risk. Likewise, a preoperative briefing can help ensure that the attending surgeon is made aware of any recent study findings. - Due to the caring style of the attending surgeon, as well as her full and early disclosure, the family only asked to be compensated for out-of-pocket expenses.
Apology and disclosure, when done in a timely and caring manner, can mitigate the damage to a patient relationship caused by an error. Patients can maintain trust and make reasonable requests for compensation when they do not believe information is being withheld or that the clinicians involved don’t care
Legal Defense Perspective
- The fact that the surgeon never was notified about the image study before the surgery fell below the standard of care.
Insurers and defense counsel will engage medical experts to review claims and determine if providers met the standard of care. A settlement is negotiated if the care in question cannot be defended..
Disposition
This case was settled in the low range < $100,000
See More MPL Cases
Medication Mix-up Contributes to Patient’s Death
Incidental Does Not Mean Insignificant
When Test Results Go Unspoken