Blog Post
MedMal Case Frequency is Down
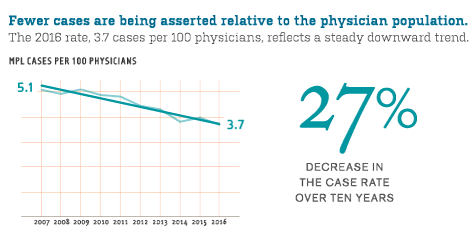
Overall MPL case frequency dropped 27 percent from 2007–2016, with an especially compelling trend for obstetrician-gynecologists.
From 2007 to 2016, the rate of medical professional liability (MPL) cases asserted per 100 physicians dropped 27%—from 5.1 to 3.7. For the roughly one million physicians across the country, this trend signals a dramatic change in their risk of being named in an MPL case. While no single factor can be aligned with an across-the-board reduction, changes in the tort environment, improved patient safety, and increasing financial risks for plaintiffs’ attorneys likely contributed.
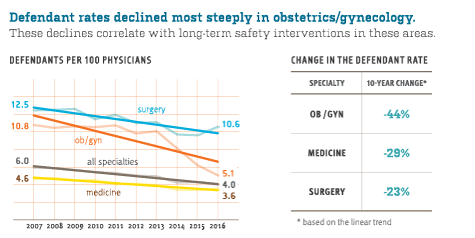
MPL experience fluctuates across legal jurisdictions and health care delivery structures, but the breadth and depth of the Candello database helps smooth variation. The downward trend in case frequency seen from 2007–2016 was universal across the many segments of health care delivery. Of course, a physician’s risk of being named in an MPL case varies considerably by clinical area of practice, but for obstetrics/gynecology and the primary sub-specialties within medicine and surgery, MPL case frequency declined steadily.
For ob/gyns (whose rate is historically higher than the average for all MDs), the risk of having an MPL case filed against them dropped 44% from 2007–2016. Such sustained results demonstrate that initiatives such as training to improve team communication during labor and delivery, and multidisciplinary education on fetal heart rate tracings, are being rewarded.
Medical subspecialties, whose case rate historically falls well below the rates for surgeons and ob/gyns, experienced a modest decline from 2007–2016. A heightened awareness of diagnosis-related trouble spots (see page 20)—and efforts to “close the loop” for test results and referrals—may be gaining traction.
The combined case rate for the surgical subspecialties, historically highest among all physicians, also declined at a modest rate (3% per year). Initiatives to reduce the risk of harm to surgery patients have aimed at pre-, intra- and post-operative vulnerabilities. Those interventions (e.g., more holistic pre-op assessment, patient-centered consent, simulation-based drills, timeouts and debriefs, and teamwork training) appear to be impacting MPL case frequency.
 |
This is an excerpt from the freely available Medical Malpractice in America. |
Related Blog Posts
Investing in Patient Safety


Mind the Gaps: Learning How to Avoid Miscommunication Pitfalls
January Safety Salute | MedStar Health Creating a Just Culture